Why Those “Little Tweaks” After Shoveling Snow Matter More Than You Think
If you live in New England, you already know — this winter has arrived with a vengeance.
After several mild seasons, we’re finally seeing the kind of snowstorms that turn everyday homeowners into part-time weightlifters overnight.
Shovels come out. Snowblowers get dragged from garages. Driveways, walkways, decks, cars, and mailboxes all need to be cleared — often quickly and in freezing temperatures.
In other words, snow removal involves a lot of lifting, twisting, pushing, and pulling, usually performed by people who haven’t done anything remotely similar in months.
So if your back feels tight, your neck is stiff, or your shoulders are aching after shoveling snow — you’re not alone. What matters most is what you do next.
Too often, people brush these symptoms off as “just soreness” or a minor tweak that will go away on its own. Maybe you take a few Advil and keep moving.
That might work short-term. But as I often remind patients at our Portsmouth, NH physical therapy clinic, the absence of pain does not mean the absence of a problem — especially when symptoms return every time you shovel, lift, or twist.
Minor stiffness or recurring tightness is often an early warning sign of a deeper mechanical issue. Over time, pain relievers stop working — or you find yourself needing them more often just to get through daily activities.
Why Clearing Snow Is a Perfect Storm for Injury
Snow shoveling injuries are incredibly common throughout New Hampshire, Maine, and Massachusetts, and for good reason.
Shoveling combines:
- Repetitive bending and spinal rotation
- Forward or overhead lifting
- Sudden force production
- Uneven, slippery footing
Snowblowers create their own challenges, including:
- Sustained pushing through heavy snow
- Resisting torque when the machine catches
- Repeated twisting to adjust the chute
- Forceful pulling to start or reposition the blower
Add cold temperatures, heavy wet snow, and muscles that aren’t warmed up, and you have a perfect setup for injury.
After every major storm here on the Seacoast, our phones start ringing. We see:
- Low back strains and disc irritation
- Neck stiffness and pain
- Shoulder injuries — especially rotator cuff flare-ups
- Knee and spine arthritis flare-ups triggered by sudden load
What makes these injuries tricky is that they don’t always show up immediately. Often it starts as:
- A dull ache
- A pinch when turning your head
- A shoulder that feels “off” when reaching
These are exactly the signs people tend to ignore — until the problem escalates.
Why “Pushing Through It” Can Backfire
One of the biggest misconceptions about musculoskeletal pain is that it has to be severe to be serious.
In reality, many long-term injuries start as small mechanical problems that were never addressed.
When you irritate a joint, disc, tendon, or nerve while shoveling snow, your body compensates. Movement patterns subtly change. Muscles tighten to protect the area.
If that irritation doesn’t resolve properly, those compensations stick around — placing stress on tissues that weren’t designed to handle it. This is how a minor tweak turns into weeks or months of pain, even after winter ends.
The Problem With Masking Pain
When pain lingers, many people look for the fastest way to quiet it:
- Anti-inflammatory medications
- Muscle relaxers
- Cortisone injections
While these options may temporarily reduce symptoms, they don’t promote healing.
Pain is information. It’s your body telling you something isn’t moving or loading properly. When you silence that message without addressing the cause, you’re more likely to repeat the same patterns — and delay true recovery.
Don’t Wait It Out — Why Early Action Matters
The good news? Most snow-related injuries respond extremely well to early, conservative care.
When addressed early:
- Recovery is faster
- Treatment is simpler
- Long-term problems are often avoided
The key is identifying what’s actually driving the pain — not just where it hurts.
Is the pain coming from the spine or the shoulder joint? Is a nerve involved? Is inflammation primary, or secondary to poor movement and overload?
At our Portsmouth, NH physical therapy and regenerative medicine clinic, we rely on repeated movement testing and test-retest methods to determine what’s truly contributing to symptoms — not just imaging findings.
Once the root cause is clear, treatment can focus on restoring movement, improving load tolerance, and supporting the body’s natural healing process.
Non-invasive options like shockwave therapy, EMTT, targeted manual therapy, and prescriptive movement work together to reduce inflammation, improve blood flow, and promote tissue healing — without masking symptoms.
Listening to Your Body Pays Off
New England winters aren’t going anywhere. Neither is snow shoveling.
If your back, neck, or shoulders still hurt days after clearing snow, that’s worth paying attention to. Pain that lingers, worsens, or changes how you move is not something to ignore.
Seeking help early doesn’t mean you’re overreacting — it means you’re being proactive.
Your body is talking to you.
The smartest move is listening now — before it starts yelling.
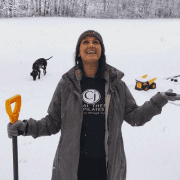
Dr. Carrie Jose, Physical Therapy Specialist and Regenerative Therapy Expert, owns CJ Physical Therapy & Pilates in Portsmouth, NH and writes for Seacoast Media Group. To get in touch or request a free discovery visit with a physical therapy specialist visit cjphysicaltherapy.com or call 603-380-7902.