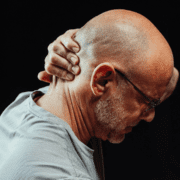
5 Signs your Headaches are coming from your Neck
Headaches impact approximately 47% of the population and are one of the most common disorders of the nervous system. If you suffer from headaches regularly, then you already know how disruptive they can be on your work life, social life, daily activities, and just overall energy and well-being.
But what makes headache management particularly challenging is how often they are misdiagnosed. The most common types of headache disorders are what’s known as primary headache disorders – and those include migraines, cluster headaches, and tension-type headaches. But you could also be suffering from a secondary headache disorder – which is caused by some other illness or physical issue. One of the most common forms of secondary headache is something called a “cervicogenic headache” – meaning it comes from your neck. They can be quite debilitating and are commonly confused with migraines – but there are some key signs to look for that make them different.
Let’s look at 4 signs that might indicate your headache is coming from your neck:
1. Headaches worsen with certain neck movements
If you find that certain movements or positions of your neck exacerbate your headaches – it could be a sign that your headaches are coming from your neck. Sometimes it’s very specific movements that trigger a headache – such as tilting your head forward or backward – or turning it from side to side. But other times it’s less obvious and related to more prolonged postures. For example, I’ve had patients experience headaches from sitting at a bar for several hours and turning their head to a certain side to talk to their friend. Pay attention to whether certain neck movements or positions create discomfort in your neck that either precedes or worsens your headache. It could mean that your headache is coming from a source in your neck.
2. Your Neck is Stiff
Another telltale sign of neck-related headaches is limited mobility or range of motion of your cervical spine (neck). If you find yourself struggling to turn your head fully, or you experience pain and stiffness when attempting to do so, it could indicate an underlying issue in your neck that is causing your headache. A common saying in my office is “mobility before stability”. If the joints in your neck don’t move fully and freely, the structures around those joints (muscles and nerves) can become angry and irritated – and this could be the source of your headaches.
3. Tenderness in your neck muscles
If you routinely have sensitivity and tenderness in the muscles of your neck – it could indicate an underlying neck problem. If you notice that your headaches seem to get triggered whenever the tension or tenderness in your neck muscles worsens – then there’s a good chance your headaches are coming from your neck. The muscles of your neck can get tense and irritated for a number of reasons – most commonly because of poor posture or because they are being overused in some capacity. Since your neck muscles have direct and intricate attachments to the base of your skull – they can be a common cause of your headaches.
4. Location of your Pain
A headache that stems from the base of your skull and stays on one side of your head – often radiating into your temple or behind your eye – is a common sign that your headache is coming from your neck. If you tend to get associated shoulder or arm pain at the same time as your headache – it’s another indicator your headache could be cervicogenic. That’s because the nerves in your neck extend into these areas and are capable of radiating pain into these locations. If you suffer from chronic headaches, pay attention to where the pain is coming from or where it’s radiation. If it’s extending beyond your head – there’s a good chance your headaches are coming from your neck.
5. Massage and Chiropractic Manipulations Help.
If you find temporary relief from your headaches any time you get a massage or see a chiropractor, it’s almost certain your headaches are cervicogenic. While it’s great you’ve found pain relief – the problem with relying on these modalities is that they are completely “passive” – meaning – you don’t have an active role in the process of relieving your headaches. Passive modalities work great when paired with specialized, corrective exercises you can do on your own that are designed to prolong the effects of these treatments. But when passive treatments are used in isolation – the headache relief tends to be short-lived. The take home point here is that if you find treatments like massage and chiropractic treatment help – your headaches are almost certainly coming from your neck.
If you suffer from debilitating headaches and haven’t yet gotten your neck thoroughly checked out as a source – you should. Because when your headaches originate from a source in your neck, it’s entirely possible to learn how to treat it and manage it naturally and on your own. But you’ll need to work with a specialist who understands cervicogenic headaches as well as the associated mechanical joint components influencing them.
Are you local to Portsmouth, NH? CLICK HERE to speak with one of my specialists for free.