6 Tips to Protect Your Back When Shoveling Snow
6 Tips to Protect Your Back When Shoveling Snow
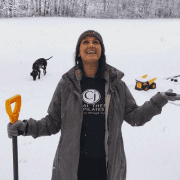
We’re finally getting some winter weather here on the seacoast. And although it’s beautiful – and the skiers are rejoicing – someone still has to shovel that snow and clear it out of the way. If that someone is you – then you’ll want to keep reading. Because repetitive bending and twisting of your back (the primary movement in shoveling) is the perfect recipe for unwanted back pain.
Here are 6 tips to protect your back when shoveling snow:
1. Warm Up First
Most people wouldn’t start a heavy workout without warming up first, yet when it comes to shoveling, we tend to just grab the shovel and go. That’s a mistake. Shoveling is a full-body activity that engages your legs, core, and upper body. If you don’t prepare your muscles, you’re more likely to strain something – especially your back.
Take five to ten minutes to warm up with light movements. Marching in place or jumping jacks help get blood flowing, while torso twists and squats loosen up your spine and legs. And don’t forget your upper body. Arm circles are a great way to warm up your shoulders – which can also get quite achy when shoveling. Taking just 10-15 min to warm up your body and lubricate your joints before shoveling can go a long way toward protecting your back.
2. Use Your Legs
Our spines weren’t designed to lift heavy things – that’s what our legs are for. Your spine’s main job is to provide structural support and stability so you can stand upright and move freely. When lifting or shoveling, your legs should be doing the work – not your back.
To ensure your legs are driving the power – it’s essential that you use proper lifting mechanics. Instead of bending or curving at your waist – hinge at your hips and bend your knees. From there, engage your hamstrings and glutes to lift the snow and use your core muscles to throw it away. Even with perfect form – your back might still get sore. That’s totally normal. But it’s far less likely to get injured – and that is what we’re trying to avoid.
3. Pivot Instead of Twist
One of the most vulnerable movements for your lower back is repetitive bending and twisting. The stress this puts on your spine makes it easy to “throw your back out.” Now let’s be clear – that doesn’t mean you should never bend or twist – your spine is designed to safely perform these motions. The problem occurs when you add load to this motion (like heavy snow) or do it repeatedly.
To protect your back – lead with your pelvis and hips instead of your torso. When turning to throw or push snow, keep your shovel and hips (use your belly button as a guide) pointing in the same direction. If they’re out of sync, it means you’re twisting from your torso instead of pivoting – and that’s a surefire way to hurt your back when shoveling.
4. Breathe to Engage Your Core
Holding your breath during exertion is common, but it can be a big problem – especially when it comes to core activation. When you hold your breath, your diaphragm can’t expand and contract properly, which is essential for engaging your deep core muscles. If your deep core isn’t firing, your larger abdominal and back muscles will struggle too.
Strengthening your core is beneficial for all activities – not just shoveling—but none of it matters if you forget to breathe. Without proper breathing, even the strongest core won’t do its job effectively, and this can set you up for a back injury over time.
5. Stay Hydrated
Even in cold weather, physical exertion can lead to dehydration. Just because you’re not sweating or feeling thirsty doesn’t mean you don’t need water. In colder temperatures, your thirst signals aren’t as strong, making it easy to overlook hydration. And even if you’re not sweating, you’re still losing fluids. Dehydration can lead to muscle fatigue, cramping, and stiffness – all of which increase your risk of a back injury while shoveling. Plus, when your muscles aren’t properly hydrated, they become less flexible and more prone to strains, making bending and lifting feel even harder.
To stay ahead of dehydration, drink water before, during, and after shoveling – even if you don’t feel thirsty. Sip small amounts frequently rather than chugging large amounts at once. Warm fluids like herbal tea or broth can help keep you hydrated while maintaining body temperature. Be mindful of caffeine and alcohol, as they contribute to dehydration. Staying hydrated keeps your muscles and joints working efficiently, making shoveling safer and easier for your whole body, not just your back.
6. Use Ergonomic Tools
Investing in an ergonomic shovel can reduce strain on your back and joints. These shovels promote better posture by minimizing bending. Many have curved handles or adjustable lengths, allowing you to maintain a more upright position. This distributes the workload more evenly, reducing stress on your back.
Now, you might be thinking, “I have a snow blower – my back will be fine.” Think again. It’s easy to push with your upper body instead of your legs, which puts strain on your spine. Poor technique makes your back more vulnerable to injury – even if you don’t feel pain in the moment. The real trouble comes later when you grab a shovel for a quick cleanup or simply sit down to relax. You may be in for a rude awakening when you stand up and realize your back is stiff and locked up. Ergonomic shovels and equipment like snow blowers go a long way in protecting you back – but they don’t replace the need for good posture and proper body mechanics.
Bonus tip: See a Specialist
If you’re already prone to back injuries and dread the thought of shoveling another snowstorm – it’s time to seek help. These tips are great for protecting a healthy back and preventing future injuries, but they won’t solve an ongoing back problem. You need expert care for that. Look for a back pain specialist who prioritizes natural solutions over pills and injections (such as a mechanical back pain specialist) so you can get back to doing all the activities you love. Oh—and shoveling too.
Are you local to Portsmouth, NH?
If so, consider speaking to one of my back pain specialists by clicking HERE.
Dr. Carrie Jose, Physical Therapy Specialist, and Mechanical Pain Expert, owns CJ Physical Therapy & Pilates in Portsmouth, NH, and writes for Seacoast Media Group. If local to Portsmouth, NH, and looking for help – request a FREE Discovery Visit with one of her Specialists by CLICKING HERE.