6 Reasons Your Muscles Are the Secret to Staying Young
When most people think about anti-aging, they picture creams, supplements, or the latest medical breakthroughs.
But one of the most powerful tools for staying young is something you’re born with – your muscles. Everyone knows muscles are key for strength and appearance, but research shows they do far more than that. Muscles act like living medicine inside your body. Every time they contract, they send out chemical signals that influence your brain, heart, bones, and immune system. In fact, researchers now recognize that maintaining muscle may be one of the most effective ways to protect your health, preserve independence, and extend your life.
So – what exactly makes building muscle such a potent anti-aging secret?
Here are six important ways your muscles act like medicine:
1. Muscles Fight Inflammation
One of the hallmarks of aging is something scientists call “inflammaging” – chronic, low-grade inflammation that damages tissues and raises the risk of cardiovascular disease, arthritis, and Alzheimer’s. But here’s what’s fascinating… When your muscles contract during exercise, they release anti-inflammatory chemicals known as myokines. One of the best studied is interleukin-6 (IL-6). Unlike the IL-6 produced by fat tissue, which fuels inflammation – muscle-derived IL-6 helps regulate the immune system and suppress harmful inflammatory signals.
This helps explain why U.S. studies, such as the long-running Alameda County Study, have consistently shown that physically active adults live longer and age with fewer health problems. In other words – every time you use your muscles – you’re helping your body reverse damaging inflammation.
2. Muscles Stabilize Blood Sugar
Muscle is the largest site of glucose disposal in your body. The more muscle you have – and the more you use it – the more efficiently your body processes sugar. Resistance training improves insulin sensitivity, which means your muscles can absorb glucose from the bloodstream more effectively.
A 2024 meta-analysis found that structured resistance training reduced HbA1c, a long-term marker of blood sugar control, by about half a percentage point – an effect comparable to some common diabetes drugs. For millions of Americans at risk for diabetes, maintaining and building muscle is one of the most powerful ways to keep blood sugar steady and prevent disease.
3. Muscles Strengthen Bones
Strong muscles don’t just move your body – they help to strengthen bone. Every time muscles contract against bone, they stimulate bone growth and increase bone density. This is one of the most effective natural defenses against osteoporosis, a disease that affects more than 10 million Americans and dramatically raises fracture risk.
As we age, fractures can mean the loss of independence. But by strengthening muscles through regular resistance training – you also strengthen the bones they attach to – creating a double layer of protection.
4. Muscles Protect Your Brain
Healthy muscles send protective signals to your brain. As previously mentioned – when you exercise and contract muscles – they release myokines. In addition to IL-6, myokines such as irisin and brain-derived neurotrophic factor (BDNF) stimulate the growth of new neurons, strengthen existing connections, and improve brain plasticity.
The benefits are measurable. Studies of older American adults have shown that maintaining muscle strength later in life is associated with sharper memory, slower cognitive decline, and reduced risk of dementia. Exercise also boosts endorphins, which elevate mood and help combat depression and anxiety. Keeping your muscles active is one of the most reliable ways to keep both your body and mind young.
5. Muscles Support Heart Health
We often think of walking or jogging as the best ways to support cardiovascular health. But research now shows that strength training deserves equal credit. Resistance exercise improves circulation, reduces arterial stiffness, and lowers blood pressure.
In a massive U.S. study of more than 116,000 adults – those who consistently met or exceeded physical activity guidelines – including strength training – had up to a 31 percent lower risk of death from any cause – and up to a 38 percent lower risk of dying from cardiovascular disease. These findings echo results from the British Journal of Sports Medicine, which showed that just 30 to 60 minutes of strength training per week reduced risk of chronic disease and early death. When it comes to your heart, strong muscles really are medicine.
6. Muscles Extend Longevity
Perhaps the most compelling evidence for the concept of “muscles are medicine” is its impact on survival. Studies consistently show that muscle mass and strength are stronger predictors of longevity than body weight or BMI. One U.S. study of college alumni found that those who maintained higher activity levels in midlife had significantly lower risks of heart disease and lived longer lives.
Muscle also serves as a critical protein reserve. When illness, surgery, or trauma strikes – your body draws on muscle stores to support healing, immune function, and tissue repair. People with greater muscle mass not only live longer but also recover more quickly when health challenges arise. Stronger muscles simply mean greater resilience.
The Bottom Line
Your muscles do far more than help you look fit or lift heavy things. They fight inflammation, regulate blood sugar, strengthen bones, protect your brain, support your heart, and extend your life. Best of all, you don’t need hours in the gym to see these benefits. Just 30 to 60 minutes of strength training per week, combined with regular movement, can produce profound results.
But if pain or injury is holding you back, don’t ignore it. The longer you wait, the harder it can be to bounce back – and the more you miss out on this natural anti-aging tool. If back, knee, hip, neck, or shoulder pain is keeping you from building muscle, talk to a physical therapy specialist who can help you return safely. With the right guidance, you can overcome those barriers and put your muscles to work – as they are your best-kept secret to staying young.
Looking for help and local to Portsmouth NH? Consider speaking to one of my specialists by clicking HERE.
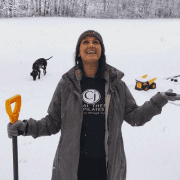
Dr. Carrie Jose, Physical Therapy Specialist and Mechanical Pain Expert, owns CJ Physical Therapy & Pilates in Portsmouth, NH, and writes for Seacoast Media Group. If local to Portsmouth, NH, and looking for help, request a FREE Discovery Visit with one of her Specialists by CLICKING HERE.